Nurses Set to Reject Pay Offer as Industrial Action Becomes More Likely
Nurses across England are expected to reject a proposed 3.6% pay rise, increasing the likelihood of potential strike action. The Royal College of Nursing (RCN) has criticised the offer as inadequate compared to settlements given to other public sector workers, and early indications suggest a strong majority of members are opposed to the deal.
While a formal decision on striking has not yet been made, turnout is believed to be high enough to meet the threshold for industrial action. The RCN is urging the government to begin discussions and has signalled a willingness to negotiate on broader issues such as pay structures, career progression, and working conditions, beyond just the headline pay figure.
The Department of Health and Social Care said that newly qualified full-time nurses would now earn £30,000 in basic salary following previous increases. However, it insisted there is no further room to move on the current pay offer, while remaining open to discussions on structural improvements across the sector.
The GMB union, which represents many NHS and ambulance workers, has also rejected the same pay award, with a clear majority of members voting against it. The union has requested urgent talks with the Health Secretary to address pay and wider concerns raised by its members.
Worlds First AI Breakthrough to Strengthen NHS Patient Safety Measures
A new artificial intelligence system is being introduced to revolutionise patient safety across the NHS, aiming to detect care issues early and prevent serious harm. The innovative tool, the first of its kind globally, will scan NHS data in near real-time to identify risks and trigger faster inspections – part of a broader move to digitise the health service under the government's 10-Year Health Plan.
The rollout begins this November, starting with a maternity care monitoring system that will flag unusual rates of stillbirth, neonatal death and brain injury across NHS trusts. This data-driven approach will enable healthcare regulators like the Care Quality Commission (CQC) to act swiftly when patterns of concern emerge, such as unexpected injuries or rising mortality rates.
The initiative supports a wider government effort to reform health and social care regulation, ensuring better outcomes for patients and faster responses to poor performance. It also marks a significant step in using technology to ease pressure on NHS staff by reducing paperwork and supporting faster, evidence-based decision-making.
Health leaders say the system will transform how safety is managed, offering earlier interventions and reducing the chances of avoidable harm. The CQC is also updating its inspection process to align with this digital shift, making assessments more responsive and transparent for both care providers and the public.
First 24/7 Community Mental Health Hub Opens in East London
A new round-the-clock mental health centre has officially opened its doors in Tower Hamlets, marking a significant milestone in the NHS’s plan to deliver more accessible, localised support. As part of the government’s 10 Year Health Plan, the centre is the first of six to roll out across England, offering walk-in care for individuals living with serious mental health conditions.
The centre brings together a wide range of services under one roof – from crisis response teams and mental health professionals to housing and employment support. Crucially, it eliminates the need for appointments or referrals, making help easier to access for those in urgent need. Staffed by a blend of NHS clinicians, peer support workers, and voluntary sector partners, it offers a joined-up approach to recovery and wellbeing.
This initiative forms part of a broader effort to move care closer to where people live, shifting away from hospital-led models. It builds on other reforms, such as the introduction of 24/7 psychiatric teams in A&E and dedicated mental health helplines across the country.
Alongside Tower Hamlets, similar hubs are planned for locations including Birmingham, Sheffield, York, Whitehaven, and Lewisham. The goal is to make community-based mental health support the norm, not the exception, ensuring people can access consistent and compassionate care whenever they need it.
New Winter Shield for Premature Babies Against RSV
Thousands of premature babies across the UK will soon benefit from a new preventative injection to guard against respiratory syncytial virus (RSV), a winter illness that can lead to severe lung infections and, in some cases, prove fatal. While many newborns gain protection through their mother’s vaccination during pregnancy, infants born before 32 weeks often miss this crucial immunity and are left highly vulnerable.
From late September, the NHS will offer a single dose of the antibody treatment Nirsevimab to around 9,000 premature and high-risk babies. Unlike vaccines that take time to build resistance, this injection delivers immediate protection lasting up to six months – just in time for the colder season when RSV spreads more rapidly.
Though RSV typically causes cold-like symptoms such as coughs and runny noses, it can lead to complications like bronchiolitis and pneumonia in vulnerable children. Data from NHS England shows premature babies are three times more likely to be admitted to hospital due to RSV and ten times more likely to require intensive care than those born at full term.
Neonatal units across the UK will administer the injection, and families of babies with heart or lung conditions or weakened immune systems will be guided by their care teams. NHS leaders hope this initiative will significantly reduce hospital admissions and protect the most fragile infants this winter.
Nature-Based Training Helps NHS Staff Bring the Outdoors into Mental Health Care
Despite many people rarely visiting parks or the countryside, the NHS is now turning to the natural world to support mental health treatment. In Sussex, healthcare professionals are taking part in a specially designed training programme that equips them to use green spaces in their day-to-day work with patients.
Backed by Natural England and delivered by community interest company Circle of Life Rediscovery, the five-month course provides hands-on experience and an accredited qualification. It’s aimed at a wide range of professionals — from therapists and social workers to psychiatrists and youth workers — and teaches how to adapt therapy practices to outdoor environments, drawing on growing evidence that time in nature can lower stress and improve physical health.
Since its launch in 2023, 36 NHS staff in Sussex have completed the training, reporting benefits not only for patients but for themselves too. Participants say they feel more relaxed and energised when working outdoors and are now applying nature-based approaches in their professional settings with the support of colleagues.
With a new round of training already underway and further sessions scheduled for 2026, this initiative is part of a broader push to understand how nature can influence health and wellbeing. A large-scale study involving 18,000 adults will track the long-term impacts of outdoor exposure on physical and mental health across the UK.
Emergency Vaccines Credited with Saving Millions of Lives and Billions in Costs
A major new study has found that emergency vaccination efforts carried out in response to outbreaks of five deadly diseases have reduced deaths by nearly 60% over the past 23 years. Covering 210 outbreaks across 49 countries between 2000 and 2023, the research highlights the impact of rapid vaccine deployment against Ebola, measles, cholera, yellow fever and meningitis.
The findings suggest that these targeted vaccination programmes didn’t just save lives but also prevented a similar number of infections, effectively curbing the scale of potential epidemics. By halting the spread early, the interventions appear to have played a key role in averting much larger public health emergencies.
In addition to the human impact, the economic benefits have been considerable. The estimated savings from avoided deaths and long-term disability equate to roughly $32 billion. However, researchers believe the true value could be far higher, as this figure doesn’t reflect the cost of managing widespread outbreaks or the economic disruption they would likely cause.
The study was supported by Gavi, the vaccine alliance, which helped coordinate many of the emergency responses. Its CEO, Dr Sania Nishtar, stressed the findings prove how vital swift vaccine roll-outs are in tackling global health threats - and why ongoing investment in vaccine initiatives remains essential.
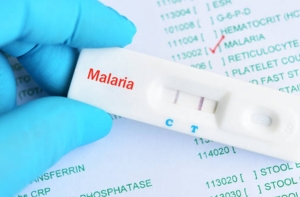
First Malaria Drug for Infants Approved, Marking Milestone in Global Health
A new malaria treatment designed specifically for newborns and very young children has received regulatory approval, marking a significant step forward in protecting the most vulnerable. The drug, created by Novartis and known as Coartem Baby (or Riamet Baby in some regions), is the first of its kind tailored for infants weighing under 4.5kg—an age group previously overlooked in malaria care.
Historically, babies have been treated with scaled-down versions of medications intended for older children, increasing the risk of incorrect dosing and adverse effects due to underdeveloped liver function. Experts have long warned of a dangerous “treatment gap” for these young patients, who are at high risk. In 2023, malaria claimed around 597,000 lives - most of them in Africa and over 75% in children under five.
The drug, approved by Swiss regulators, is expected to be introduced across African nations within weeks, following successful trials involving eight countries. Novartis says it will distribute the medicine primarily on a not-for-profit basis to ensure accessibility.
Health leaders and researchers have hailed the development as a game-changer. Dr Marvelle Brown of the University of Hertfordshire emphasised that this breakthrough could drastically reduce malaria-related deaths among babies - especially those with sickle cell disease - while promoting more equitable access to life-saving care.
Starmer Unveils Bold NHS Overhaul Focusing on Local Care and Prevention
Labour leader Sir Keir Starmer has revealed a wide-ranging 10-year strategy aimed at transforming healthcare in England, shifting emphasis from hospitals to community-based services. The plan includes the creation of around 50 neighbourhood health centres within the current parliament, with a long-term goal of 300 by 2035. These hubs, staffed by a mix of medical professionals, are designed to offer accessible, localised treatment and reduce hospital overload.
A major digital push will see the NHS app upgraded, allowing patients to access their complete medical records, book appointments, and manage prescriptions. Starmer described it as having a “24/7 doctor in your pocket”. However, concerns remain about accessibility for those without smartphones, particularly older individuals.
Preventative health is another key focus, with proposals to tackle obesity through reward-based schemes modelled on a Singaporean initiative. Participants could earn digital NHS points for healthy choices, which may be redeemed in shops and restaurants. There are also plans to expand access to weight loss services and introduce clearer alcohol labelling.
Mental health and dentistry also feature, with dedicated emergency departments for psychiatric care and reforms aimed at tackling the shortage of NHS dentists. However, critics note the plan lacks a direct strategy for the struggling social care sector, which many believe is essential to fully restoring the NHS.
Major NHS Shake-Up as Hundreds of Oversight Bodies to Be Axed
The government has announced plans to scrap over 200 organisations involved in managing and monitoring the NHS in England, as part of efforts to simplify the health system. Among those set to close are Healthwatch England, which champions patient rights, and the National Guardian’s Office, which supports whistleblowing within health services. Health Secretary Wes Streeting described the current structure as overly complicated, saying it’s time for “more action, less oversight”.
This overhaul forms part of Labour’s upcoming 10-year vision for healthcare. The move will see bodies created under previous governments, including local health planning groups, dissolved. The government argues that the sheer number of agencies has resulted in conflicting guidance that burdens staff and slows down progress. Ministers say greater focus will be placed on patient feedback through the NHS app in future.
The changes have prompted mixed reactions. While some, including NHS Confederation chief Matthew Taylor, welcomed the chance to cut duplication and invest more in frontline care, there are concerns that vital protections could be lost. Healthwatch England’s chief executive expressed sadness but pledged to ensure patients’ voices remain heard during the transition.
A pilot scheme is also planned linking hospital funding to patient ratings, with poor feedback potentially diverting funds into improvement initiatives. Leaders warn such measures must be carefully designed to avoid unfairly penalising hospitals for issues beyond their control.
Primary School Pupils Learn Sun Safety to Cut Skin Cancer Risk
Young children across Kent are taking part in a new scheme teaching them how to stay safe in the sun, with the aim of lowering rates of skin cancer in future generations. The pilot project, set to roll out nationally in PSHE lessons from 2026, encourages children as young as five to check UV levels and apply sunscreen correctly. Melanoma, the most dangerous type of skin cancer, is strongly linked to UV rays. Experts warn that sunburn in early life greatly increases the chance of developing the disease later on.
Figures from Cancer Research UK show that 18,300 people were diagnosed with melanoma in 2021, with numbers expected to rise to over 21,000 by 2026. Michelle Baker from the Melanoma Fund, the charity leading the initiative, said teaching children sun-safe habits early on could help reduce these cases. “We want to empower children to protect themselves — it’s their superpower,” she explained.
At Platt Primary School in Maidstone, pupils are learning about UV indexes, sunscreen application, and the importance of sun protection. Headteacher Emma Smith said the children have responded enthusiastically, adding that early education helps them resist unhealthy influences as they grow.
Experts stress there is no such thing as a safe tan, as tanning indicates skin damage. To stay protected, children should stay in the shade between 11am and 3pm, wear hats and cover up, and use sunscreen with at least SPF 30 and good UVA protection.